Bruce Willis’ family recently announced that the 67-year-old actor was diagnosed with a progressive neurodegenerative disease called frontotemporal dementia (FTD). It helped explain how his condition had changed since he retired a year ago.
“Unfortunately, communication issues are just one symptom of the illness Bruce is facing,” his family said in an official statement released in February. “It’s heartbreaking, but I’m relieved to finally have a definite diagnosis.”
Last week, Willis’ wife, Emma Heming-Willis, explained how the family is learning to navigate dementia care. Learning how to cope with the inevitable progression of disability is basically a major lifeline that loved ones and caregivers of people with FTD must grapple with. Scientists are now studying people with FTD or at risk of developing the disease to better understand what’s going on in the brain. is in clinical trials.
Although less common than certain other neurodegenerative diseases such as Alzheimer’s and Parkinson’s, FTD is the most common form of dementia in people under the age of 60. It tends to develop earlier than other dementias. However, FTD usually develops between the ages of 40 and 60. An estimated 60,000 people are affected in the United States alone.
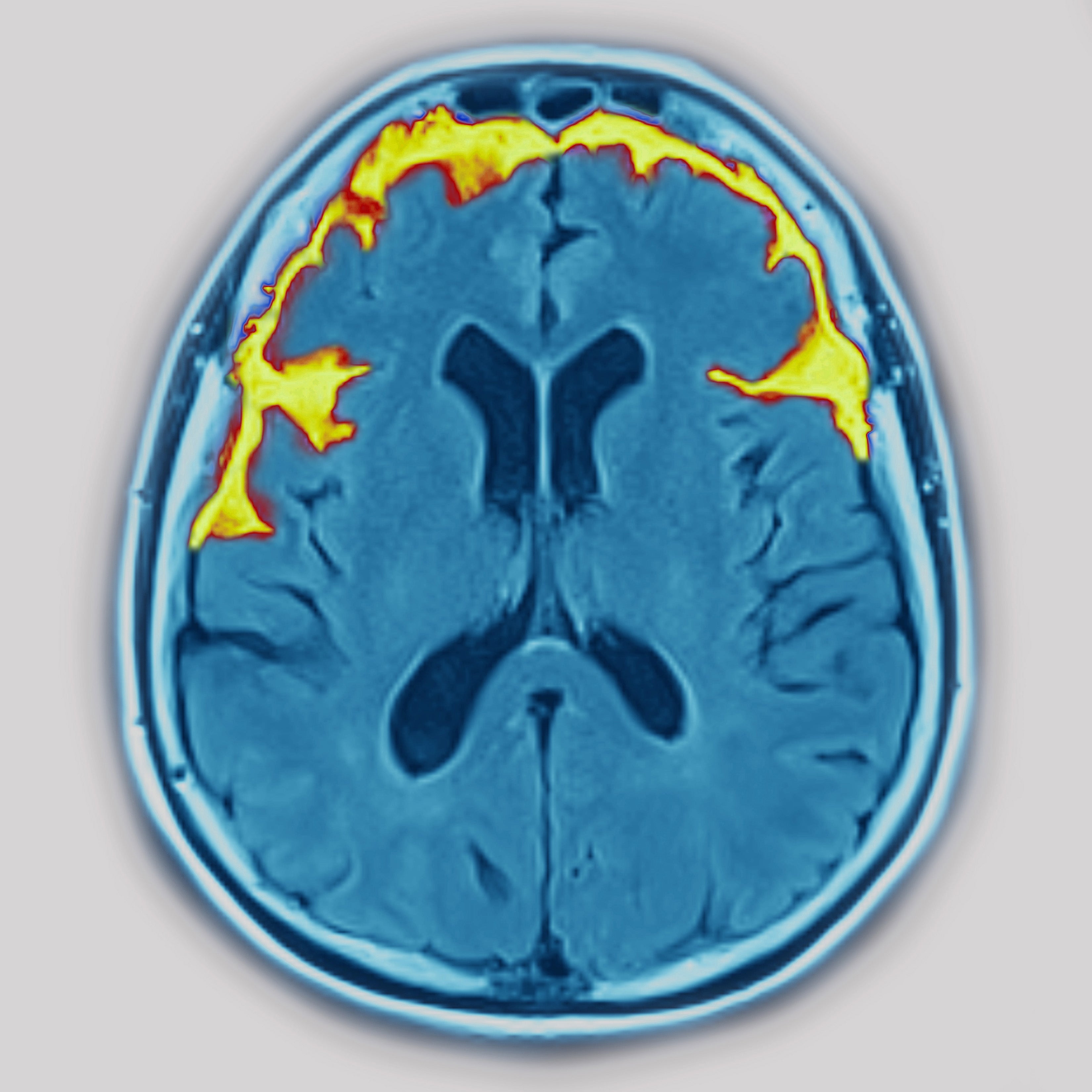
The term FTD refers to a range of disorders that affect the frontal and temporal lobes of the brain (regions associated with personality, behavior, language, and other high-level brain functions). The disease can be devastating for FTD patients and their spouses, children or grandchildren, says Elizabeth Finger, a neurologist and professor at Western University in Ontario. One of the most insidious aspects of FTD is that it seems to suddenly change someone’s personality.
“Physically, you may be fine for a while, so it’s like having strangers living with you in your family,” says Finger. “It helps if the family gets a diagnosis because they often live with a feeling of alienation for a while. will be.”
What are the symptoms of FTD?
FTD has several variant. Each is characterized by a set of symptoms related to where in the brain the disease begins. Behavioral variants associated with changes in the frontal and temporal lobes are the most common. It includes symptoms such as apathy, blunted emotions, impulsiveness, and decision-making and judgment problems.
Variants associated with changes in language ability are known as primary progressive aphasia and usually involve the dominant frontal and temporal lobes (for most people, these are on the left side of the brain). There are three main subtypes of these variants: semantic, non-fluent, and logpenic he. Semantic subtypes mainly lead to loss of word comprehension. An affected person’s vocabulary diminishes over time, making it increasingly difficult to read, write, and understand dialogue. People with the non-fluent subtype have difficulty speaking but retain the meaning of words. In the early stages of this subtype, words may be difficult to pronounce and slurred. In advanced stages, they may stop speaking altogether. People with the log-decreasing variant have trouble finding the right words during conversation.As the disease progresses, these people may have trouble understanding complex sentences.
Movement disorders are the most prominent symptom of other variants. This can occur when FTD co-occurs with amyotrophic lateral sclerosis (ALS). ALS is a neurodegenerative disease that leads to progressive loss of neurons involved in movement.
All of these variants overlap to some degree, according to neurologist Yolande Pijnenburg, a professor at the University of Amsterdam Medical Center. “The syndromes are most distinct when they are in their initial state,” she says.
find out the cause
FTD is commonly associated with loss of neurons in the frontal and temporal lobes of the brain. But what caused that loss? Postmortem examination of the FTD patient’s brain revealed that the condition was primarily associated with abnormal accumulation of two proteins in her, tau and her TDP-43. Both of these are also believed to be involved in Alzheimer’s disease. Scientists have found other proteins that may be responsible for FTD, but tau and he say that alterations in TDP-43 account for more than 90% of his total, Johns said of Hopkins University. says neuropsychiatrist Chiadi Onyike.
Studies suggest that genetic mutations cause FTD in about one-third of affected individuals. A dozen mutations have been associated with this condition, the most common appearing to be in specific genes that cause abnormal accumulation of tau and TDP-43.
But scientists know very little about what causes the disease in the other two-thirds of affected people without the genetic disorder, the so-called sporadic FTD. The only risk factor that has yet been identified is a history of concussion or traumatic brain injury, says Finger. But that alone explains only a small part of the risk, she adds. This is because the majority of FTD patients have not experienced such brain damage, and most who have had them have not developed her FTD.
know the signs
According to Pijnenburg, diagnosing FTD presents several challenges. It now takes an average of 3.6 years for people to receive an accurate diagnosis of the condition. Most people with FTDs, especially behavioral variants, are unaware that changes are occurring and rarely seek medical help on their own. Another possible explanation is the disease or another mental health condition. Importantly, Pijnenburg says there is a relative lack of public awareness of the disease.
A definitive FTD diagnosis is only possible if researchers perform postmortem brain examinations, Finger notes, or if a person carries a so-called autosomal dominant mutation.
However, there are other tools for evaluating FTD, including neurological and psychiatric evaluation, neuroimaging, genetic screening, and analysis of personal medical history. Neuroimaging techniques such as magnetic resonance imaging and positron emission tomography can reveal signs indicative of her FTD of brain damage and dysfunction. Genetic screens can identify her FTD-associated mutations in a subset of people with FTD. According to Pijnenburg, these techniques can pinpoint anywhere between his 74% and his 93% of FTD cases.
Researchers around the world are now studying asymptomatic people with genetic mutations associated with FTD. This is an attempt to understand how the disease develops and potentially help develop treatments, including treatments that slow, stop or prevent the disease.
In Canada and several European countries, a research consortium called the Genetic Frontotemporal Dementia Initiative (GENFI) is conducting studies tracking more than 1,000 people with FTD-related genetic mutations. . Jonathan Lawler, a neurologist at University College London and GENFI coordinator, said the group is trying to determine how to detect early changes in asymptomatic individuals considered at risk. Now, 10 years into the study, Rohrer says previous behavioral and brain pathological observations suggest that subtle changes in cognition and brain structure can precede the onset of symptoms by many years. It says it shows something.
In 2019, GENFI formed the Frontotemporal Dementia Prevention Initiative (FPI) in collaboration with researchers based in the United States, Australia, and several countries in Asia, South America, and Africa, Rohrer said. says. The team involved is pooling data to create an international registry of her FTD study participants who can be enrolled in clinical trials. Ultimately, a global research effort plans to set up clinical trials for treatments that might prevent people from developing FTD symptoms.
testing new treatments
Studies of people with genetic forms of FTD have already led to a variety of potential disease-modifying treatments, some of which are being tested in clinical trials. Includes Phase 3 trials. Progranulin is a multifunctional protein whose decreased levels in the FTD lead to accumulation of her TDP-43. Trials of therapeutics aimed at restoring or attenuating the activity of known FTD-associated mutated genes are also underway.
Scientists hope that if these treatments work, they may be used to help people with sporadic FTD. “There is a growing belief in the field that genetic forms of therapy may be translatable into sporadic forms,” says Finger.
But before that happens, Rohrer points out, scientists need to overcome another major obstacle to treating sporadic FTD. It is to identify biomarkers such as biomarkers that can reveal tau or TDP-43 protein in blood or spinal fluid to determine which pathological processes. playing.
There are now ways to manage and treat certain FTD symptoms. One important aspect of care today is family and caregiver education. Other approaches include psychotherapy and pharmacological interventions targeting specific behavioral or cognitive symptoms and speech disorders. Physical or occupational therapy can address language and movement problems, but lifestyle or environmental changes (limiting driving or using credit cards, maintaining a quiet environment, structured routines, ) can help with behavioral symptoms. Researchers are also beginning to look at ways to improve brain function, says Onyike. For example, combining brain stimulation with speech therapy for people with aphasia.
Although disease-modifying treatments are not yet available, researchers see some promise in recent treatment advances. “We are optimistic and moving forward,” he says Onyike. “Ten years ago clinical trials were about drugs to reduce symptoms or boost cognition. Today they stop neurodegeneration and rehabilitate the brain.”